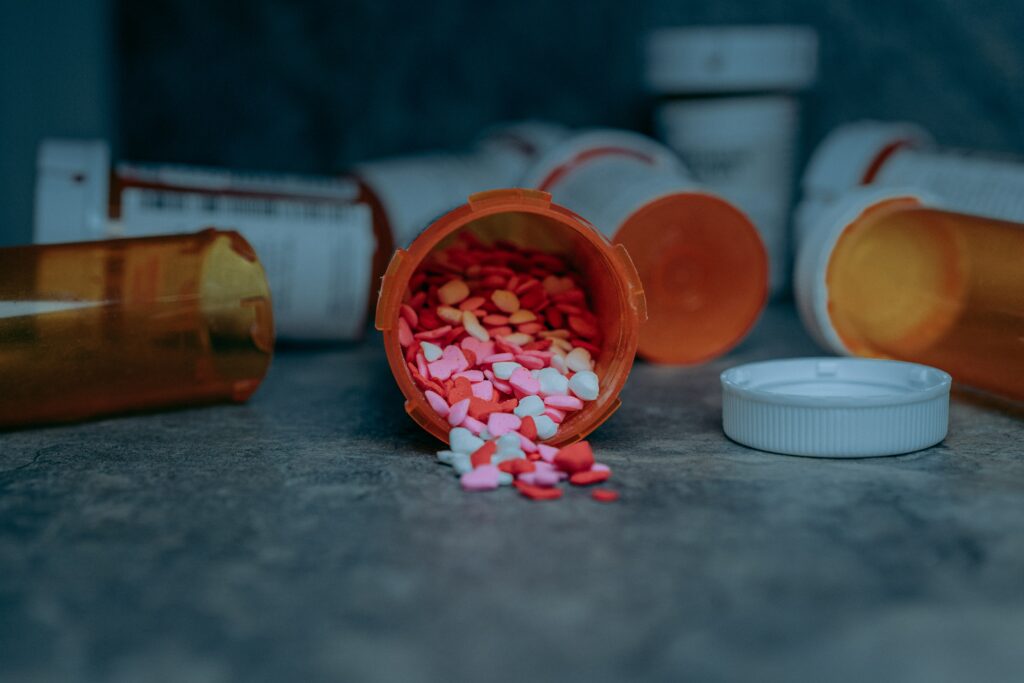
It is widely believed that substance abuse and addiction in the elderly is a hidden epidemic. Even if they have no history, it should be taken seriously as substance abuse, especially in the elderly, can exacerbate health problems. In 2016, 19.3% of older adults in the United States filled at least one opioid prescription, and 7.1% had four or more opioid prescriptions that year.
Due to the changes that come with aging, substance abuse can have a disproportionately negative affect on older adults. Chronic illnesses or pain are often treated with potentially addictive medications. Further, the elderly metabolize medications slower, making them more sensitive with higher impairments that decrease memory, balance and may cause serious falls.

Elderly substance abuse is underrecognized in older adults due to:
- Social Isolation: Living alone and away from family may increase use without anyone to see the issue growing.
- Ageism: May lead to the belief that older adults have earned certain indulgences.
- Quality of Life: Includes concerns about living with pain.
Oxycodone (Percocet and OxyContin), hydrocodone (Vicodin), codeine, morphine, and fentanyl—are commonly prescribed for severe or chronic pain. Benzodiazepines such as diazepam (Valium), lorazepam (Ativan), alprazolam (Xanax), midazolam (Versed) function as relaxers. Both are highly addictive. Some signs of addiction include:
- Hiding prescriptions.
- Running out of medications quickly.
- Showing withdrawal symptoms (e.g., nausea, vomiting).
- Signs of cognitive impairment and decreased balance/falls.
- Using multiple pharmacies to fill prescriptions.
Acknowledging there is a problem is the first step to helping them overcome it and develop a plan. Open up a discussion about what pain management alternatives they have tried and help them talk with their doctor to see if there is a way you can work together to manage the situation.


